Apple Watch’s blood oxygen level and coronavirus: interpretation and explanations
A pulse oximeter has been added to the Apple Watch Series 6. But what do your results actually mean? Do they mean that you have coronavirus? This article explains it all.
Note that this article, though written by a doctor, does not replace seeking the assistance of a medical professional if you have concerns about your health.
As a doctor who likes tech, I’ve always been excited when the Apple Watch comes out with new health functions like the ECG function and now the blood oxygen app. But I feel as if there needs to be some understanding of how to interpret them, because it may mislead people into thinking they’re not at risk for coronavirus, when in reality the only way you are really able to tell is to get tested with a swab.
We use pulse oximetry all the time for patients. The peripheral oxygen saturation - also known as the SpO2 - is a critical vital sign that, well, tells us how well oxygenated is in your blood. The new Apple Watch Series 6 now comes with one. It works by basically using the lights on the watch to reflect how “red” the blood is in your body. The more red that reflects back to the watch, the more oxygen your blood has.
But it’s important how to understand how to interpret the readings that you find. Note that Apple provides an explicit statement that “Blood Oxygen app measurements are not intended for medical use, including self-diagnosis or consultation with a doctor, and are only designed for general fitness and wellness purposes. If you have questions about your health, contact a medical professional.”

A normal fit human being will generally have an SpO2 above 95%. So even if it’s 96% or 97%, it indicates that there’s nothing wrong from an oxygenation perspective - though if you have symptoms like chest pain, you may still actually have something very wrong going on. It is an isolated result and needs to be expertly interpreted with a doctor’s advice.
If the oxygen saturation starts to dip to 94% or below, it might suggest impaired oxygenation. There’s a very wide variety of conditions that cause your oxygen saturation to go down. Most commonly, conditions that affect the lung - like asthma, COPD, or pulmonary embolism - would be the main culprits. Some people who have chronic lung conditions (particularly COPD) tolerate lower levels of SpO2 after having had their body adjust to it over long periods of time: so a 70 year old man with COPD who has an oxygen saturation of 93%, may at another moment have an oxygen saturation of 95%, and you wouldn’t necessarily worry too much about that 93% unless he had other symptoms. Fundamentally however, if any actual symptoms occur - like shortness of breath, chest pain, or dizziness - you should see a doctor immediately.
The question that’s probably on everyone’s mind is: how does the Apple Watch blood oxygen level relate to whether you have coronavirus or not? To understand that, you have to understand how to grade severity of Covid-19.
COVID-19 can be mild, moderate, or severe. Mild cases can generally stay at home under self isolation, whereas moderate or severe cases may need hospital.
Mild coronavirus = normal blood oxygen levels (>95%), but not worse. But a normal oxygen level does not rule out coronavirus.
Most people who contract Covid-19 will either be asymptomatic or mildly symptomatic. They may have symptoms that are extremely difficult to tell from a standard common cold - sore throat, runny nose, a bit of a cough, fevers - but importantly, those with mild CoVid-19 (and no other medical conditions) will not have low blood oxygen levels.
So just because you don’t have a low blood oxygen level SpO2 <95%, does not mean that you don’t have Covid-19. In other words: you can have a normal blood oxygen and still have CoVid. A normal oxygen level does not rule out coronavirus. It just means that if you do have coronavirus, it is more likely to be considered a mild version.
Generally speaking, most people who have only mild COVID-19 should be managed at home under self-isolation, and no further investigations - apart from the swab that’s required for initial diagnosis - is necessary, unless other medical conditions are being considered. Your doctor may recommend that, if you have asthma or COPD, that you use an additional amount of puffer medication compared to usual. 4 out of 5 people with COVID-19 will have a
mild illness and will usually recover 2 to 3 weeks after the initial onset of
symptoms (source). If respiratory symptoms do worsen, this is most likely to occur in the 2nd or 3rd week of illness. For some patients, symptoms may persist for longer than 4 weeks, or new symptoms may develop. The range of potential long term symptoms of COVID-19 is as yet unknown.
Moderate or severe coronavirus
Shortness of breath, however, is a sign you should be worried about. Shortness of breath does not appear in mild coronavirus infections, but if you have shortness of breath, it indicates — if you have coronavirus — then that coronavirus is either moderate or severe. In this circumstance, seek medical advice.
Following the current evidence based guidelines we have in Australia (by the National Covid-19 Clinical Evidence Taskforce), moderate illness is classified as thus:
Stable adult patient presenting with respiratory and/or systemic symptoms or signs. Able to maintain oxygen saturation above 92% (or above 90% for patients with chronic lung disease) with up to 4 L/min oxygen via nasal prongs. Characteristics: prostration, severe asthenia, fever > 38 ̊C or persistent cough, clinical or radiological signs of lung involvement, no clinical or laboratory indicators of clinical severity or respiratory impairment.
And severe coronavirus illness is defined as such:
Adult patients meeting any of the following criteria: respiratory rate ≥ 30 breaths/min, oxygen saturation ≤ 92% at a rest state, arterial partial pressure of oxygen (PaO2)/ inspired oxygen fraction (FiO2) ≤ 300
That’s a lot of jargon there. But the takeaway points for adults are:
- If you have viral symptoms but your oxygen saturation is above 95%, it does not mean that you don’t have coronavirus, it just means that you either have something that’s not coronavirus or you have a mild form of coronavirus.
- If your blood oxygen levels are below 92% on your Apple Watch and you do not have a pre-existing lung condition or you have significant symptoms, seek medical advice immediately.
- If you have a previous lung condition and your blood oxygen levels are below 90% on your Apple Watch, seek medical advice immediately.
If any of the following symptoms occur, you need to seek medical attention immediately as you may need to go to hospital:
• severe shortness of breath or difficulty breathing
• blue lips or face
• pain or pressure in the chest
• cold, clammy or pale and mottled skin
• new confusion or fainting
• becoming difficult to rouse
• little or no urine output
• coughing up blood
How do I interpret my Apple Watch blood oxygenation levels for children?
For kids, the criteria is somewhat similar at the time of writing (17/9/2020). In mild illness, the child should not have a SpO2 of less than 92%. If the blood oxygen level is less than 92% in a child, or they look like they’re having trouble breathing, seek medical attention. If you have any concerns at all, a low threshold for seeking the advice of a doctor is warranted.
How reliable is the Apple Watch in detecting oxygen levels?
It can’t always detect oxygen levels. To directly copy and paste from Apple’s website itself:
Even under ideal conditions, your Apple Watch may not be able to get a reliable blood oxygen measurement every time. For a small percentage of users, various factors may make it impossible to get any blood oxygen measurement.
- Skin perfusion (or how much blood flows through your skin) can impact measurements. Skin perfusion varies significantly from person to person and can also be impacted by the environment. If you are out in the cold, for example, the skin perfusion in your wrist might be too low for the sensor to work with the Blood Oxygen app to get a measurement.
- Permanent or temporary changes to your skin, such as some tattoos, can also impact performance. The ink, pattern, and saturation of some tattoos can block light from the sensor, making it difficult for the Blood Oxygen app to get a measurement.
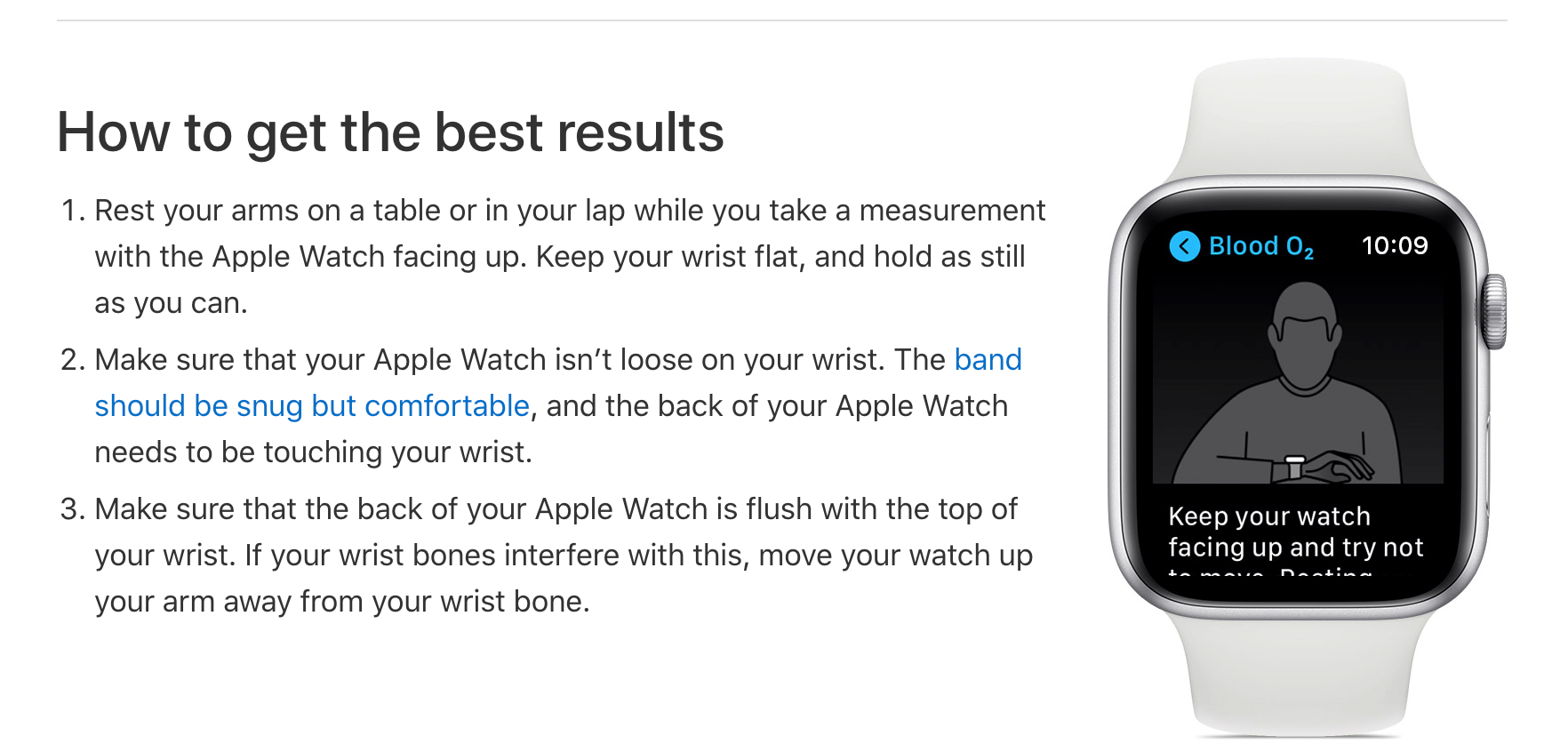
- Motion is another factor that can affect your ability to get successful background or on-demand measurements. Certain postures, such as arms hanging by your side or fingers in a fist position will also result in unsuccessful measurements.
- If your heart rate is too high (above 150 bpm) while at rest, you won't be able to get a successful blood oxygen measurement.
It’s also important that you make sure that the Apple Watch is flush with your wrist, as this will also affect results.
References
- https://covid19evidence.net.au/ - Covid-19 Taskforce Guidelines (for medical professionals).
- https://support.apple.com/en-au/HT211027
Disclaimer
Although I’m sure I have, if I haven’t iterated the point enough: don’t make a self-diagnosis, seek a doctor’s advice on how to proceed.
If any mistakes or you'd like to get in contact with me, please do so at david (at) dabido.com.au. You can use the contents from this article freely for your own articles, but just leave a link back to this site on your article if you do - thanks!
